by Thomas D. Giles, MD
Introduction
As epidemiologic and clinical data regarding the relationship between blood pressure (BP) and the risk for cardiovascular disease (CVD) have accumulated, a pronounced shift has taken place in how the disease of hypertension is viewed and defined. Cardiovascular (CV) risk has been found to be elevated at BP levels previously considered normal; in some cases, sporadic elevations in BP levels may be physiologically benign and not associated with additional CVD risk.[1-3] As a consequence, many hypertension experts consider elevated BP at its core a disease marker, rather than a cause of hypertension. Moreover, elevated BP, as 1 marker of CVD, frequently coexists with other equally compelling disease markers.[2] Elevated BP should not, therefore, be viewed or treated in isolation, but considered in the context of whole patient care, which takes into account the presence of other risk factors and disease markers for CVD to achieve a more comprehensive, or global, assessment of CV risk.
With these points in mind, in 2005, the Hypertension Writing Group (HWG), a national group of hypertension specialists, proposed a new definition of hypertension as "a progressive cardiovascular syndrome, the early markers of which may be present even before BP elevations are observed."[4] The stated goal of the new definition was to identify individuals at risk for CVD at an earlier point in the disease process, as well as to avoid labeling persons as hypertensive who are at low risk for CVD.[4] Viewed from this perspective, the HWG believed that threshold-based classification systems of hypertension, such as that endorsed in the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7),[5] while serving as tools to identify patients across a broad range of CVD risk, may lead to underestimation or overestimation of clinical risk within individual patients. In either case, the presence or absence of other disease markers or risk factors, the coexistence of target-organ damage, or both can be used to risk-stratify patients with hypertension more accurately.
To simplify risk stratification and align it more closely with clinical practice, the HWG proposed classifying all patients as either normal or hypertensive (eliminating the prehypertension category proposed in JNC 7), with hypertension classified into stage 1, stage 2, or stage 3.[4] Because the CV syndrome represented by hypertension may be present even when BP falls within the normal category by conventional standards, the risk categories created by the HWG focus not on BP levels per se, but on the presence of deleterious BP patterns or the presence of CVD. Stages of hypertension are further categorized based on the presence of risk factors for early, advanced, or progressive CVD, as well as by other CVD markers (classified as BP, cardiac, vascular, renal, and retinal changes) and target-organ damage (classified as cardiac, vascular, renal, and cerebrovascular).[4]
Beyond the goal of providing a more clinically relevant assessment of global CV risk in clinical practice, this paradigm shift served to focus attention on the enormous unmet need regarding prevention and optimal treatment of hypertension across a spectrum of fields, from basic research and drug development to patient education and clinical management.[4] Two critical areas of research in particular -- the development of specific and sensitive cost-effective tests that can detect early CVD markers in the clinical setting, and the development of strategies to slow or prevent the onset of target-organ damage or overt CVD by treating early vascular derangements -- may benefit from being examined within the context of the categories for hypertension.
Recently, the HWG further refined and updated the definition and classification of hypertension.[6] This article reviews the revised definition and classification scheme and the implications for clinical practice. As the authors stressed, however, while definitions of disease are useful for detection, management, research, and education, definitions alone do not constitute recommendations for treatment. In the latter case, the initiation of treatment should be individualized and guided by CV risk, rather than BP thresholds.[1]
Blood Pressure as a Biomarker for Hypertension
The concept of elevated BP as a disease marker for hypertension, rather than its cause, is supported by multiple lines of evidence suggesting that the risk for renovascular and CV sequelae may be higher than expected in the presence of normal or near-normal BP in some patients, or, conversely, lower than expected in the presence of above-normal BP in others. This view is based, in part, on the physiologically dynamic nature of BP, in which tissue perfusion is matched with metabolic demands in a complex, ever-changing manner that depends on the coordinated activity of numerous mechanisms involved in hemostasis, including the sympathetic nervous system, the renin-angiotensin system, and the vasodilatory system (eg, prostaglandins and nitric oxide).[4] According to this perspective, optimal BP can vary among individuals and within the same person, depending on hemodynamic circumstances. Sporadic BP elevations may occur in individuals who have no evidence of early CVD.[2] Conversely, because adverse CV and renal outcomes increase across all BP values, hypertension-related morbidity and mortality can occur even at BP levels considered normal by conventional standards. The significant proportions of myocardial infarctions and strokes that occur in patients who have only slight BP elevation, or even normal BP, adds weight to this argument.[7]
Perhaps the most convincing evidence against using BP thresholds to define hypertension is that there is no threshold of BP above 115/70 mm Hg that identifies CV risk -- that is, risk is linear and doubles for each 20/10 mm Hg increase in BP.[2] As a consequence of the dynamic nature of BP, it may be more clinically relevant to use BP patterns, rather than discrete BP thresholds as measured in the clinic, when assessing CV risk in an individual patient. Thus, the HWG places particular attention on ambulatory BP and the contribution of systolic BP (SBP) and pulse pressure (the difference between SBP and diastolic BP [DBP]) to risk, because these are widely considered to be more accurate markers of CV risk than is office DBP, particularly in older patients.[5,8]
The Interrelationship of High Blood Pressure and Other Cardiovascular Risk Factors
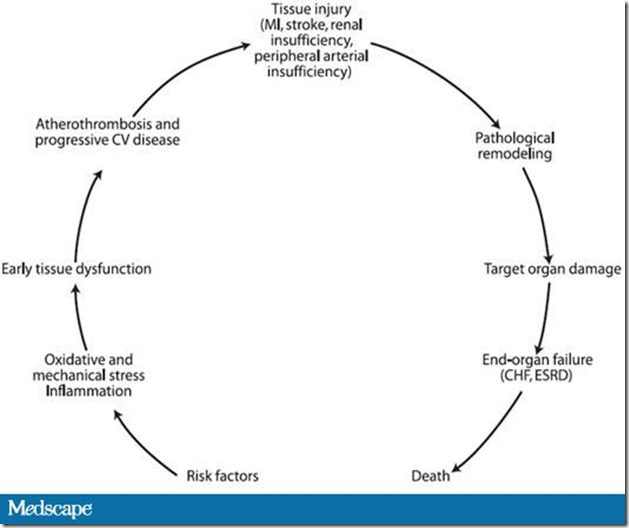
Another key principle endorsed by the HWG is that of the interrelationship between elevated BP and other CV risk factors. Even in patients with frank elevations in BP, risk stratification based on BP levels alone often underestimates CV risk. This is because above-optimal BP levels rarely occur in isolation, and patients seen in clinical practice frequently have multiple CVD markers or risk factors (eg, overweight, insulin resistance, dyslipidemia) that point to greater overall risk.[1,9-13] What is particularly significant, from the perspective of defining hypertension beyond BP thresholds, is that many of these disease processes are intimately interrelated and interact via common pathobiologic processes involving oxidative stress and endothelial dysfunction (Figure).[14] Moreover, the presence of risk factors and disease markers defines the earliest stage in this CVD continuum, well before overt CVD and target-organ damage can be measured in the clinic.[14] From this perspective, above-optimal BP (a risk factor) is not necessarily synonymous with hypertension (a disease representative of progressive CVD and tissue injury).[6]
Figure. Cardiovascular and renal pathophysiologic continuum. CV = cardiovascular; MI = myocardial infarction; CHF = congestive heart failure; ESRD = end-stage renal disease. Adapted from Dzau VJ, et al.[14]
Another consequence of the CV and renal pathophysiologic continuum is that the complex interplay of risk factors and disease markers frequently may manifest as a dramatically higher CV risk than would be expected, based on thresholds for each individual risk factor alone. This is highlighted by the particularly deleterious condition known as the cardiometabolic syndrome, in which individual risk factors combine to increase CV risk synergistically, rather than additively.[12,15] Ultimately, a more clinically meaningful assessment of CV risk can be obtained by global assessment of a patient's risk, rather than focusing solely on whether a patient has crossed a particular BP threshold.
Taken together, this evidence suggests that it may be more useful to view BP as 1, but not the only, biomarker for the disease hypertension, and to view above-optimal levels of BP in an individual patient as those that, when sustained, cause damage to the vasculature.[6] This forms the basis of the revised definition of hypertension, as shown in Table 1.
Table 1. Revised Definition of Hypertension From Hypertension Writing Group 2009
| • Hypertension is a progressive CV syndrome arising from complex and interrelated etiologies |
| • Early markers of the syndrome are often present before BP elevation is sustained; therefore, hypertension cannot be classified solely by discreet BP thresholds |
| • Progression is strongly associated with functional and structural cardiac and vascular abnormalities that damage the heart, kidneys, brain, vasculature, and other organs, and lead to premature morbidity and death |
| • Reduction of elevated BP generally confers a reduction in the risk for CV events. Note that HWG separates elevated BP (one manifestation of the disease) from hypertension (the disease) |
BP = blood pressure; CV = cardiovascular
From Giles T, et al.[6]
Because hypertension is defined by as "a progressive cardiovascular syndrome," it is clinically helpful to categorize, or stage, patients (Table 2), with each stage characterized by the cumulative presence or absence of markers of hypertensive CVD and evidence of target-organ damage. This provides a snapshot of the extent to which the disease has advanced at a particular time.[6]
Table 2. Revised Definition and Classification of Hypertension From Hypertension Writing Group 2009
| Classification | Normal | Stage 1 Hypertension | Stage 2 Hypertension | Stage 3 Hypertension |
| Descriptive category | Normal BP or rare BP elevations AND no identifiable CVD | Occasional or intermittent BP elevations OR early CVD | Sustained BP elevations OR progressive CVD | Marked and sustained BP elevations OR advanced CVD |
| Cardiovascular risk factors (see Table 3) | None or few | Several risk factors present | Many risk factors present | Many risk factors present |
| Early disease markers (see Table 4) | None | Usually present | Overtly present | Overtly present with progression |
| Target-organ disease (see Table 5) | None | None | Early signs present | Overtly present with or without CVD events |
BP = blood pressure; CVD = cardiovascular disease
From Giles T, et al.[6]
In the broadest sense, individuals are classified as either normal or hypertensive based on their CV status (ie, the absence or presence of identifiable CVD), regardless of their BP pattern. The stages within the hypertension category are further refined, based on BP patterns or the extent of CVD (early, advanced, or progressive). Each hypertension stage is further characterized by the cumulative presence or absence of risk factors for CVD (Table 3);markers of hypertensive CVD, such as microalbuminuria or mild left ventricular hypertrophy (Table 4); and evidence of target-organ damage, such as frank albuminuria or moderate-to-severe left ventricular hypertrophy (Table 5).[6] The occurrence of a major cardiac event clearly places the progression of hypertensive CVD at a more advanced stage.[6]
Table 3. Cardiovascular Risk Factors
| Increasing age |
| Elevated BPa |
| High heart rate |
| Overweight/obesity |
| − Increased BMI |
| − Central obesity |
| − Increased abdominal circumference |
| − Increased abdominal adiposity (waist-to-hip ratio)a |
| Dyslipidemia |
| − Elevated LDL or non-HDLb cholesterol |
| − Low HDL cholesterola |
| − Elevated triglyceridesa |
| Elevated blood glucose, insulin resistance, or diabetes mellitusa |
| Chronic kidney disease |
| Smoking |
| Family history of premature CVD (age < 50 yr in men, < 60 yr in women) |
| Sedentary lifestyle |
| Psychosocial stressors |
| Elevated hs-CRP |
BMI = body mass index; BP = blood pressure; CVD = cardiovascular disease; HDL = high-density lipoprotein; hs-CRP = high-sensitivity C-reactive protein; LDL = low-density lipoprotein
aComponents of the metabolic syndrome
bNon-HDL cholesterol = total cholesterol minus HDL cholesterol
Table 4. Early Markers of Hypertensive Cardiovascular Disease
| System | Physiologic Alteration |
| Blood pressure | |
| Loss of nocturnal BP dipping | |
| Exaggerated BP responses to exercise or mental stress | |
| Salt sensitivity | |
| Widened pulse pressure | |
| Cardiac | |
| Left ventricular hypertrophy (mild) | |
| Increased atrial filling pressure | |
| Decreased diastolic relaxation | |
| Increased natriuretic peptide | |
| Renal | |
| Microalbuminuria (urinary albumin excretion of 30-300 mg/day)a | |
| Reduced estimated GFR (60-90 mL/min) | |
| Cerebrovascular | |
| Stroke | |
| Transient ischemic attack | |
| Decreased cognitive function | |
| Dementia | |
| Loss of vision |
BP = blood pressure; GFR = glomerular filtration rate
aAlso a marker of microcirculatory disease
Table 5. Hypertensive Target-Organ Damage and Overt Cardiovascular Disease
| System | Evidence of Target-organ Damage and Cardiovascular Disease |
| Cardiac | |
| Left ventricular hypertrophy (moderate to severe) | |
| Systolic or diastolic cardiac dysfunction | |
| Symptomatic heart failure | |
| Myocardial infarction | |
| Angina pectoris | |
| Ischemic heart disease or prior revascularization | |
| Vascular | |
| Peripheral arterial disease | |
| Carotid arterial disease | |
| Aortic aneurysm | |
| Renal | |
| Albuminuria (urinary albumin excretion > 300 mg/day) | |
| Chronic kidney disease (estimated GFR < 60 mL/min) or ESRD | |
| Cerebrovascular | |
| Stroke | |
| Transient ischemic attack | |
| Decreased cognitive function | |
| Dementia | |
| Loss of vision |
ESRD = end-stage renal disease; GFR = glomerular filtration rate
Clinical Characteristics and Practical Implications of the Proposed Hypertension Categories
A practical clinical interpretation of the revised hypertension categories is shown in Table 6.
Table 6. Clinical Characterization, BP Patterns, and Practical Implications of the Hypertension Algorithm
| Hypertension Category | Clinical Characterization | BP Pattern | Practical Implications |
| Normal | Optimal BP levels | Resting BP levels usually < 120/80 mm Hg | Includes some patients identified as having prehypertension (based on JNC 7 criteria) |
| No identifiable early markers of CVD | Occasional BP elevations, even to ≥ 140/90 mm Hg, may occur | ||
| Stage 1 | Early CVD markers present | BP levels > 115/75 mm Hg | Earliest identifiable stage of hypertensive disease |
| Frequently 1 or more CVD risk factors present | BP may be frankly elevated, particularly with environmental stress | Includes individuals with prehypertension (based on JNC 7 criteria) who also have CVD risk factors or early disease markers | |
| No evidence of target-organ damage | |||
| Stage 2 | Diffuse disease markers present OR evidence (limited) of early target-organ damage | Sustained resting BP frequently ≥ 140/90 mm Hg, with much higher elevations induced by physiologic or psychologic stressors | Equivalent to JNC 7 stage 1 hypertension |
| Indicates progressive disease | |||
| Risk factors, if not attenuated, continue to contribute to progressive target-organ disease | |||
| Stage 3 | Overt CVD present | Sustained resting BP levels ≥ 140/90 mm Hg usual (untreated or inadequately treated) | Equivalent to JNC 7 stage 2 hypertension |
| Marked BP elevations to levels > 160/100 mm Hg not uncommon (untreated or inadequately treated) | Includes all individuals with clinical evidence of overt target-organ damage or CVD, or who have sustained a CVD event, regardless of BP levels |
BP = blood pressure; CVD = cardiovascular disease; JNC 7 = Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure
In the algorithm, individuals with optimal levels of BP and no identifiable early markers of CVD are categorized as normal. These individuals usually have resting BP levels of 120/80 mm Hg or lower, but BP may be elevated occasionally, even to levels of 140/90 mm Hg or higher.[6] Given the limits of clinic BP measurements, home BP determinations or 24-hour ambulatory BP recordings may be helpful in identifying patients with more than occasional BP elevations, who may be categorized more appropriately as having stage 1 hypertension.[16]Because the HWG algorithm does not recognize a prehypertension category, some individuals designated as having prehypertension according to the JNC 7 classification may be considered normal in the paradigm.
The earliest identifiable stage of hypertensive disease, stage 1 hypertension, is characterized by the presence of early CVD markers. Although BP levels are higher than 115/75 mm Hg and may be frankly elevated in patients at this stage, abnormal BP patterns -- including loss of nocturnal dipping, exaggerated responses to exercise or mental stress, and widened pulse pressure -- may provide clearer evidence of the presence of early hypertensive disease.[4] Although patients should have more than 1 CV risk factor to be included in this category, they should not have any evidence of target-organ damage.
In contrast to stage 1, stage 2 hypertension is characterized by diffuse disease markers and evidence of progressive disease as a consequence of persistent functional and structural changes in BP control mechanisms and in the heart and vasculature. Although patients at this stage frequently have sustained elevations in resting BP levels of 140/90 mm Hg or higher -- with much higher elevations induced by physiologic or psychologic stress -- it is important to recognize that any individual with numerous disease markers or limited evidence of early target-organ damage, such as left ventricular hypertrophy, fits into this category, regardless of BP levels. Methods of detecting or measuring some of the early target-organ damage characteristic of this stage of hypertension are currently limited to specialized or research settings, and further evaluation is needed to determine their potential utility and cost-effectiveness in clinical settings.[6] Nonetheless, aggressive management of CV risk factors that are identified in patients at this stage may help attenuate the progression of target-organ damage.
Finally, stage 3 hypertension is an advanced stage of the hypertensive continuum, characterized by the presence of overt CVD. Overt hypertensive target-organ disease is often pervasive, and CVD events may have already occurred. If inadequately treated or left untreated, individuals at this stage usually have sustained resting BP levels of 140/90 mm Hg or higher, although marked elevations to levels higher than 160/100 mm Hg are not uncommon.[6] Regardless of BP levels, however, all individuals with clinical evidence of overt target-organ damage or CVD, as well as those who have already sustained CVD events, are included in this category. Reaching this phase means that damage to target organs, as well as overt cardiorenal disease, has already occurred. As a consequence, CV risk factor modification and treatment of target-organ disease and all identified CVD should be vigorous and sustained.[6]
Strategies for and the Clinical Implications of Treating Patients Along a Continuum of Global Cardiovascular Risk
The paradigm shift in viewing elevated BP as a marker for hypertension and hypertension as a progressive CVD syndrome has important implications for treating patients in the clinical setting. The risk-based approach proposed by the HWG will lead to reclassifying patients who were previously designated prehypertensive (based on JNC 7 criteria) to either HWG normal or stage 1 hypertension.[4] In terms of treatment, lowering BP remains an important goal of antihypertensive therapy, yet ultimately the overarching objective is to prevent CV complications.[9] Treatment of other CV risk factors is therefore equally important. Moreover, CV risk factors, including elevated BP, are not only precipitators, but also continuous pathogenic components at every stage of progression of CVD.[9] Clinical strategies, therefore, need to focus on detecting and treating patients at risk at every stage along the continuum, from preventing target-organ damage and interrupting CVD progression in patients with early-stage hypertension, to making aggressive efforts to slow further disease progression and avoid CV events in patients with late-stage hypertension.
Evidence for the benefit of antihypertensive treatment in early-stage hypertension (HWG stage 1 or JNC 7 prehypertension category) has only recently become available. The Trial of Preventing Hypertension (TROPHY) study has shown that antihypertensive therapy may help prevent the development of elevated BP levels among individuals with BP lower than 140/90 mm Hg who are at high risk for frank hypertension (due to the presence of multiple CV risk factors).[17] In line with the HWG paradigm, patients in this study had high-normal SBP/DBP levels of 130-139/85-89 mm Hg at baseline, yet had a strikingly high rate of CV risk factors other than elevated BP.[17] Among the TROPHY patients, 96% had at least 1 additional CV risk factor, includingvarious measures of dyslipidemia, insulin resistance, and obesity, as well as elevatedhematocrit and heart rate; 81% had 2 or more additional risk factors; and33% had 4 or more additional risk factors. The most prevalent risk factor in thecohort as being overweight.[2,17] Patients were randomized to receive treatment with the angiotensin receptor blocker candesartan or placebo for 2 years, followed by an additional 2 years of placebo-only therapy; all patients were instructed to make changes in lifestyle to reduce BP throughout the trial.[17] After 2 years, hypertension haddeveloped in 154 patients in the placebo group and 53 patients in the angiotensin receptor blockergroup, representing a significant 63% relative risk reduction with pharmacotherapy (P < .001). After 4 years, hypertension had developed in 240 patients assigned to placeboand 208 patients assigned to active treatment (relative risk reduction, 15.6%;P < .007). Serious adverse events occurred in 3.5% of patients who received active treatment and in 5.9% of those who received placebo. As the authors noted, the absolute difference between active treatment and placebo at 2 years in TROPHY, 26.8%, is much higher than the 8% absolute difference observed in the Trials of Hypertension Prevention,[18] the only trial of lifestyle modification with a similar duration, suggesting that drug therapy plus lifestyle modification is more effective than lifestyle modification alone in early hypertension.[17]
The benefit of treatment with antihypertensive agents in patients classified as normotensive by conventional standards also is supported by the Perindopril Protection Against Recurrent Stroke Study (PROGRESS).[19] In this study, antihypertensive treatment in subjects without elevated BP (mean BP, 136/79 mm Hg) but with a history of target-organ damage -- in this case, a history of transient ischemic attacks or stroke -- was associated with a significant 27% reduction in the relative risk for stroke compared with placebo (P < .01), similar to the 32% reduction observed in patients designated as hypertensive.[19] Moreover, intensive BP reduction with combination therapy was associated with better outcomes than less-intensive BP reduction with single-agent therapy, regardless of hypertension status. Because individuals similar to those considered normotensive in PROGRESS would be classified as having stage 2 hypertension (based on the presence of target-organ damage) in the HWG paradigm, results of this study highlight the importance of considering comprehensive risk factor assessment, including the presence of target-organ damage, when defining and staging patients with hypertension.
Whether all individuals with early-stage hypertension, as defined by the HWG, should be treated with antihypertensive therapy requires further study. As the group emphasized in their 2005 report, characterizing hypertension as a complex CV disorder associated with, but not exclusively defined by, high BP is best viewed as a transitional strategy that is intended to generate further clinical research into improved strategies for detecting, treating, and possibly preventing the disease.[4]
Summary
The key points advanced by the HWG in their updated hypertension position paper are that BP serves as a biomarker for the disease hypertension and, as such, elevated BP is not synonymous with hypertension. Some individuals may exhibit elevated BP in the absence of hypertension, whereas other individuals with the same levels of BP might be classified into different stages of hypertension.[6] Therefore, for purposes of calculating total CV risk and staging patients as normal or hypertensive, BP should be evaluated in the context of other CV risk factors and disease markers. Ultimately, it is hoped that the risk-based approach to defining and staging hypertension, as proposed by the HWG, will lead to earlier identification of individuals with hypertensive CVD. Preliminary data, such as that described by the TROPHY Investigators, suggest that lowering BP with pharmacologic therapy can prevent or delay the progression of hypertensive CVD even at early stages (ie, HWG stage 1 hypertension/JNC 7 prehypertension). Additional research is necessary to confirm these findings and identify cost-effective methods to detect and measure early CVD markers in clinical practice.
This activity is supported by an independent educational grant from Pfizer.
This article is a CME certified activity. To earn credit for this activity visit:
http://cme.staging.medscape.com/viewarticle/708548
References
- Weir MR. Risk-based classification of hypertension and the role of combination therapy. J Clin Hypertens (Greenwich). 2008;10:4-12.
- Giles TD. Assessment of global risk: a foundation for a new, better definition of hypertension. J Clin Hypertens (Greenwich). 2006;8:5-14.
- Khosia N, Black HR. Expanding the definition of hypertension to incorporate global cardiovascular risk. Curr Hypertens Rep. 2006;8:384-390.
- Giles TD, Berk BC, Black HR, et al. Expanding the definition and classification of hypertension. J Clin Hypertens (Greenwich). 2005;7:505-512.
- Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560-2572.
- Giles TD, on behalf of the Hypertension Writing Group. Definition and classification of hypertension: an update. J Clin Hypertens (Greenwich). In press.
- Sierra C, de la Sierra A. Early detection and management of the high-risk patient with elevated blood pressure. Vasc Health Risk Manag. 2008:4;289-296.
- Franklin SS, Khan SA, Wong ND, et al. Is pulse pressure useful in predicting risk for coronary heart disease? The Framingham Heart Study. Circulation. 1999;100:354-360.
- Basile J. Management of global risk across the continuum of hypertensive heart disease. J Clin Hypertens (Greenwich). 2006;8:21-30.
- Khot UN, Khot MB, Bajzer CT. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA. 2003;290:898-904.
- Neaton JD, Wentworth D; the Multiple Risk Factor Intervention Trial Research Group. Serum cholesterol, blood pressure, cigarette smoking, and death from coronary heart disease: overall findings and differences by age for 316,099 white men. Arch Intern Med. 1992;152:56-64.
- Meigs JB, D'Agostino RB Sr, Wilson PW, et al. Risk variable clustering in the insulin resistance syndrome: the Framingham Offspring Study. Diabetes. 1997;46:1594-1600.
- Gregg EW, Cheng YJ, Cadwell BL, et al. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA. 2005;293:1868-1874.
- Dzau VJ, Antman EM, Black HR, et al. The cardiovascular disease continuum validated: clinical evidence of improved patient outcomes: Part I: pathophysiology and clinical trial evidence (risk factors through stable coronary artery disease). Circulation. 2006;114:2850-2870.
- Hoerger TJ, Ahmann AJ. The impact of diabetes and associated cardiometabolic risk factors on members: strategies for optimizing outcomes. J Manag Care Pharm. 2008;14:S2-S14.
- Pickering TG, White WB; American Society of Hypertension Writing Group. ASH position paper: home and ambulatory blood pressure monitoring. When and how to use self (home) and ambulatory blood pressure monitoring. J Clin Hypertens (Greenwich). 2008;10:850-855.
- Julius S, Nesbitt SD, Egan BM, et al; Trial of Preventing Hypertension (TROPHY) Study Investigators. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N Engl J Med. 2006;354:1685-1697.
- The Trials of Hypertension Prevention Collaborative Research Group. Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure: the Trials of Hypertension Prevention, phase II. Arch Intern Med. 1997;157:657-667.
- PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001;358:1033-1041.



0 comments:
Post a Comment